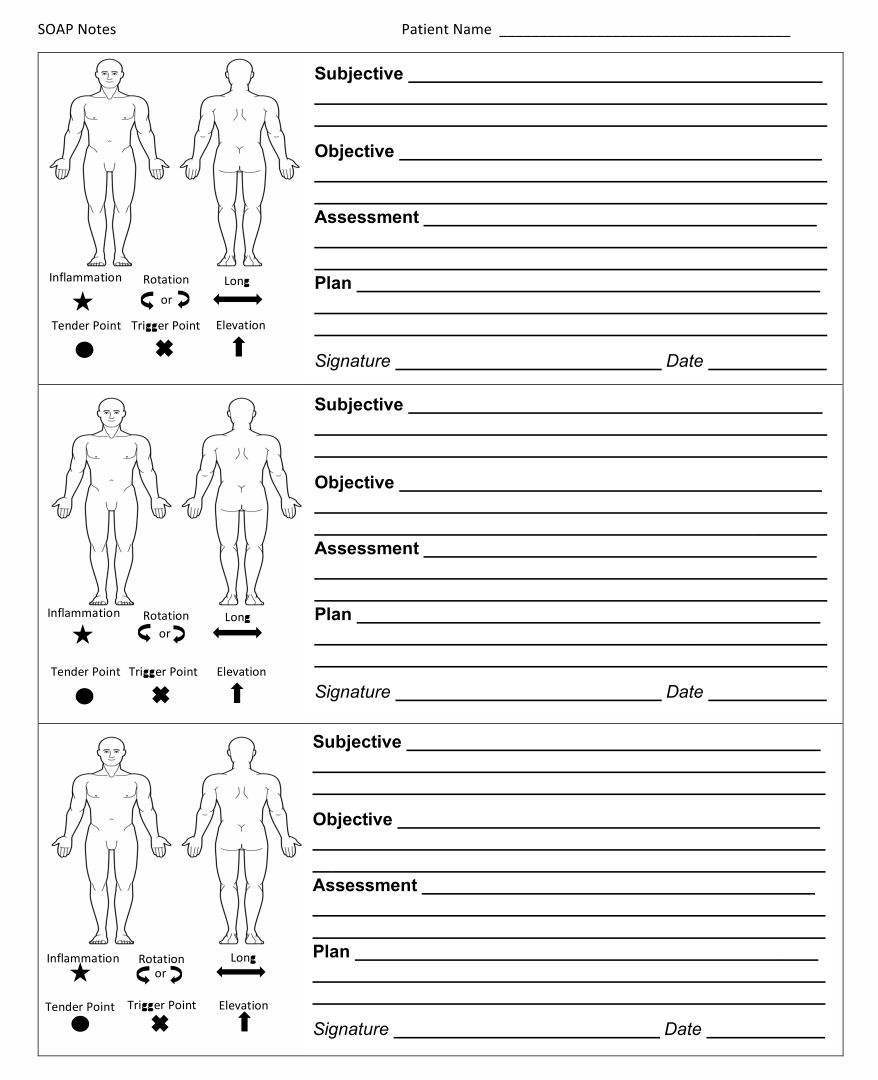
Using printable counseling SOAP note templates streamlines your documentation process, allowing you to efficiently record sessions, observations, assessments, and plans.
This not only saves time but also ensures that your notes are organized and consistent, improving the quality of care you provide to your clients. With these templates, you can quickly reference past sessions, making it easier to track progress and tailor your counseling strategies to meet your clients' needs effectively.
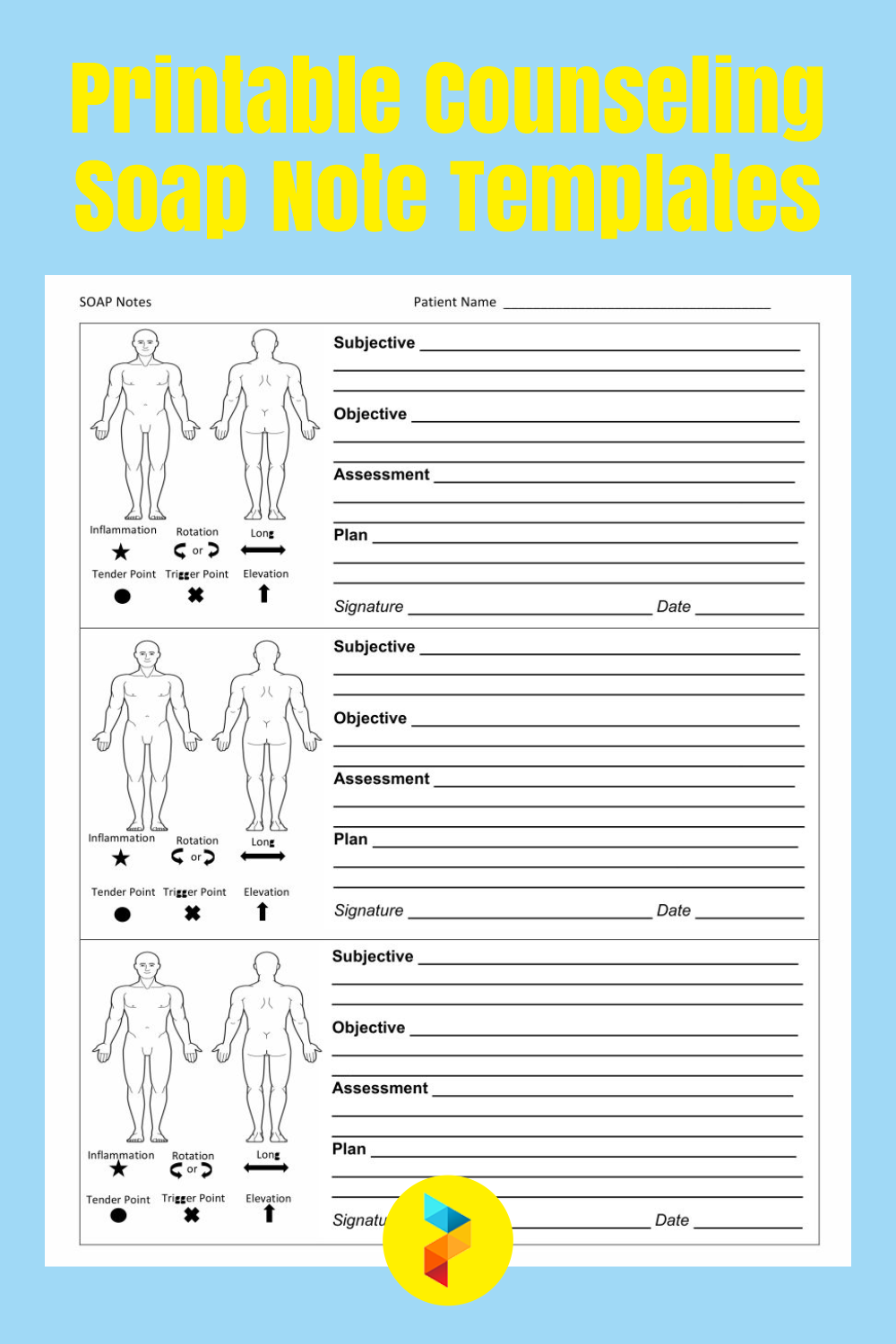
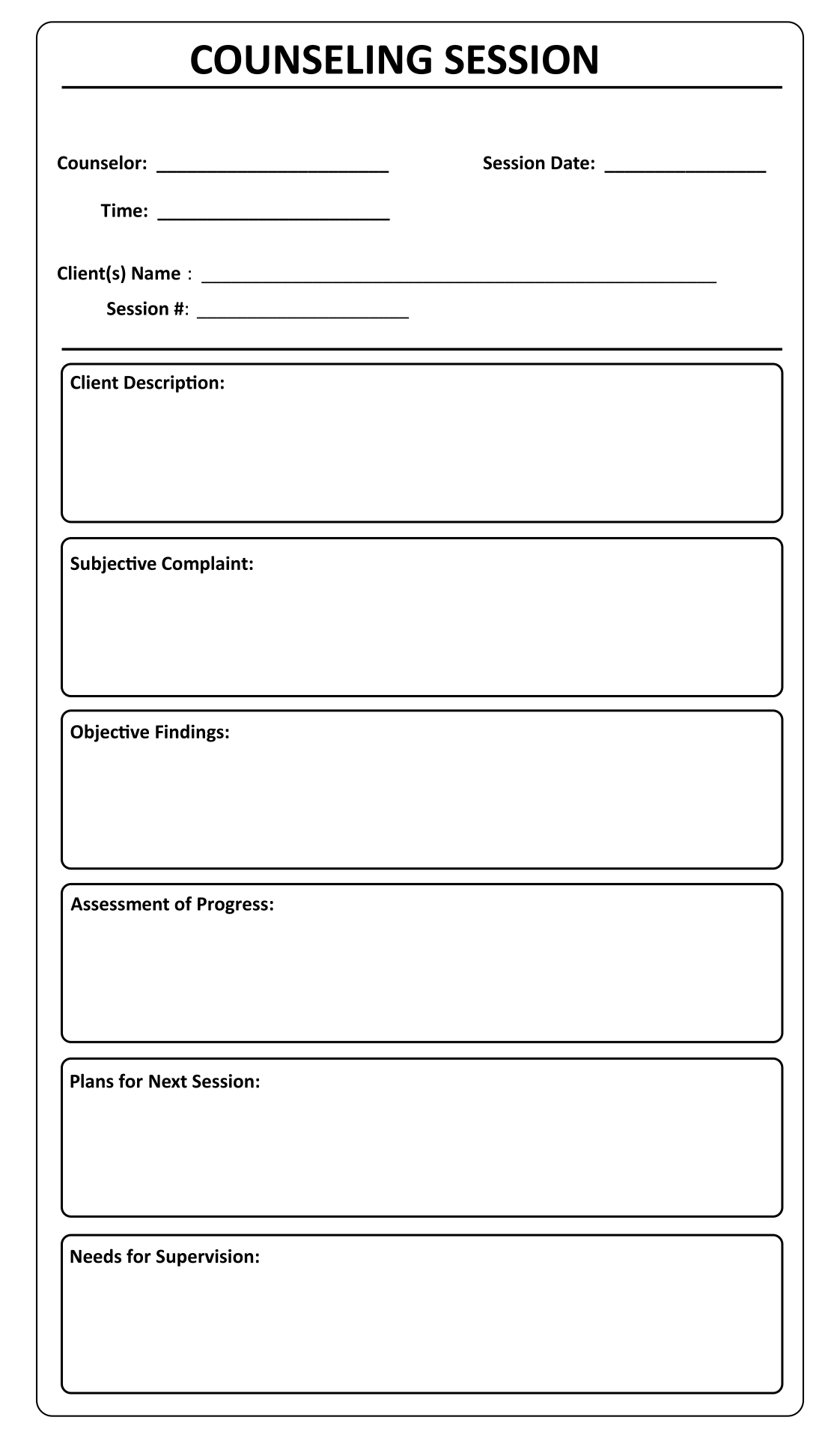
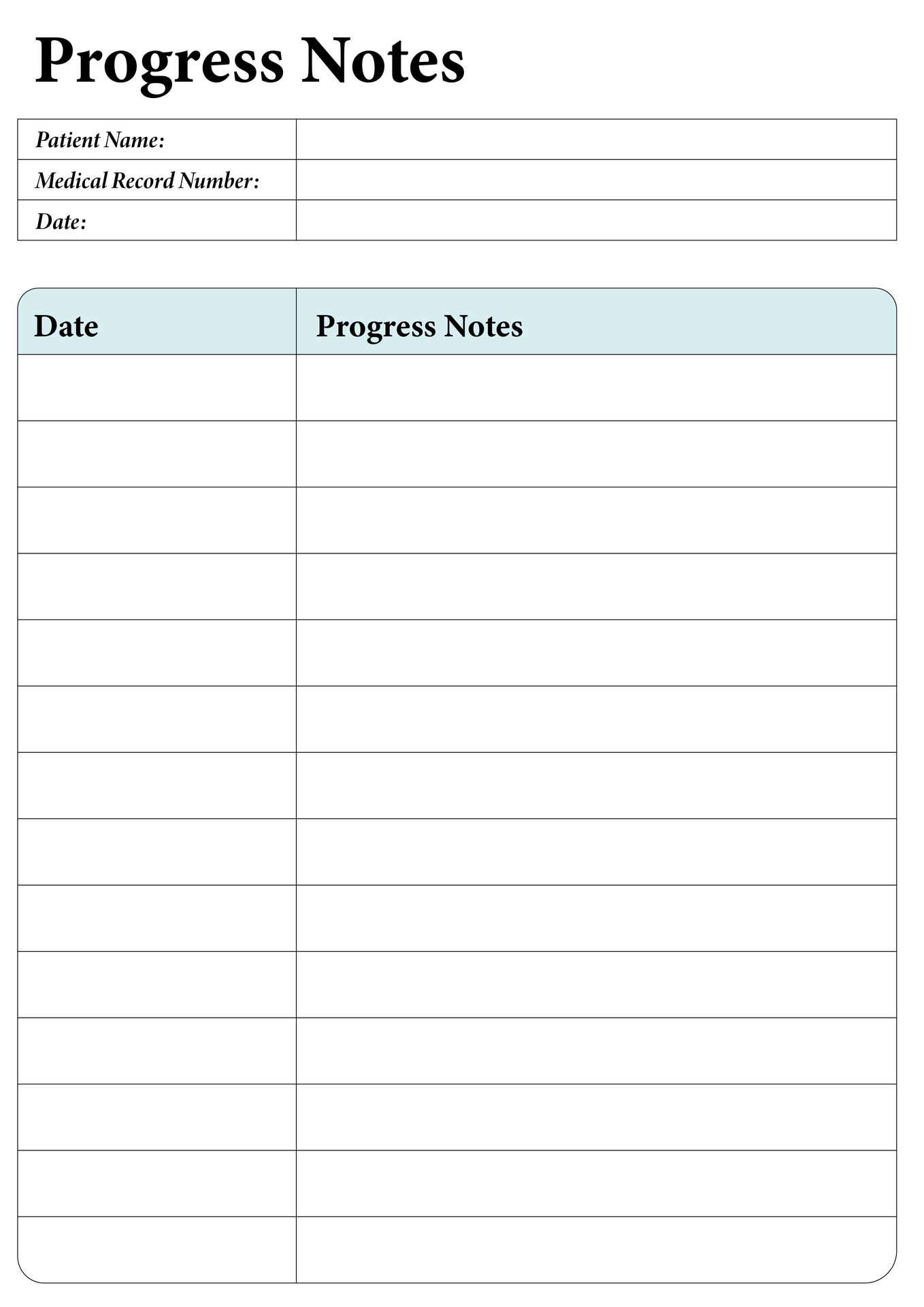
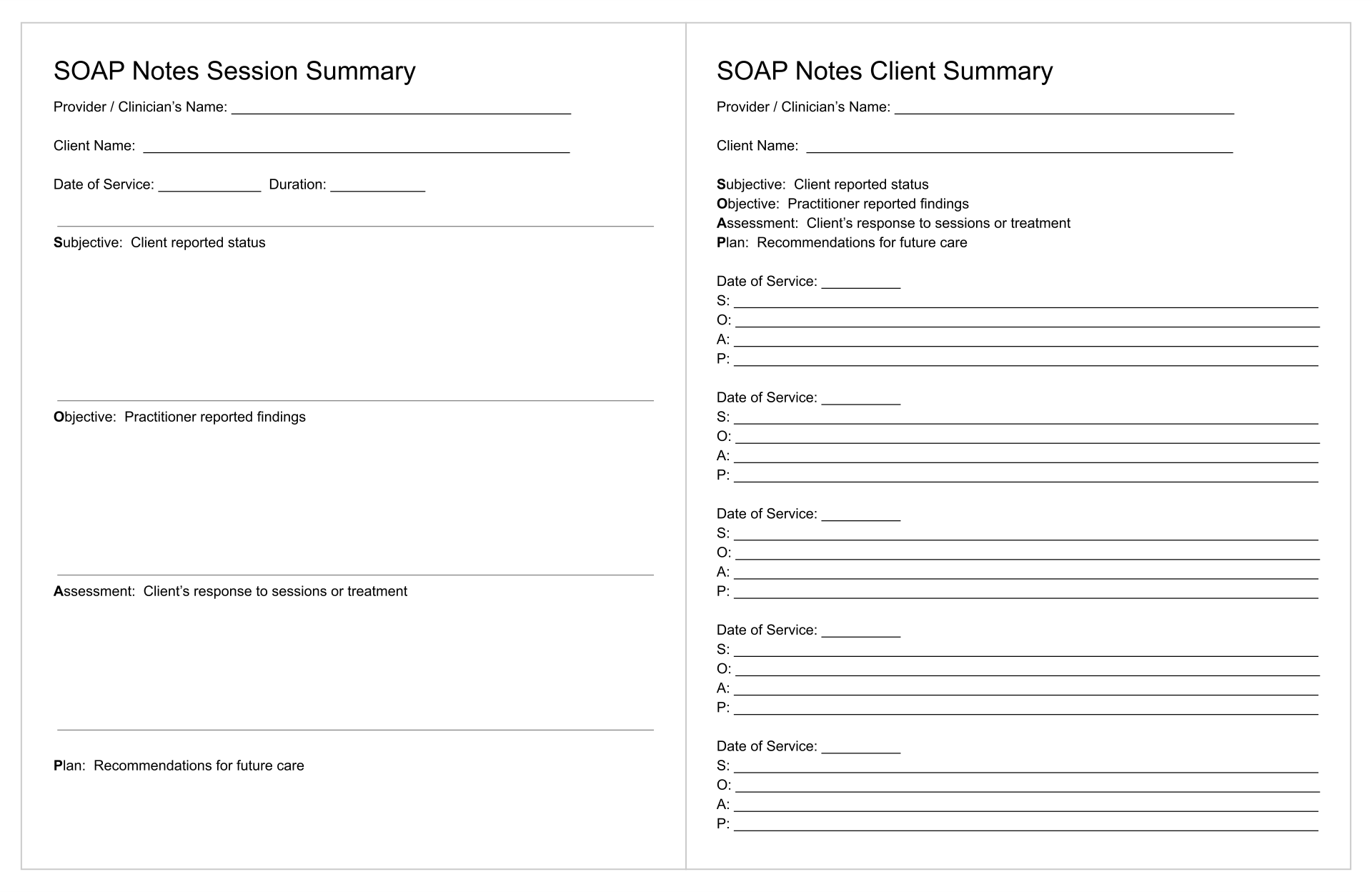
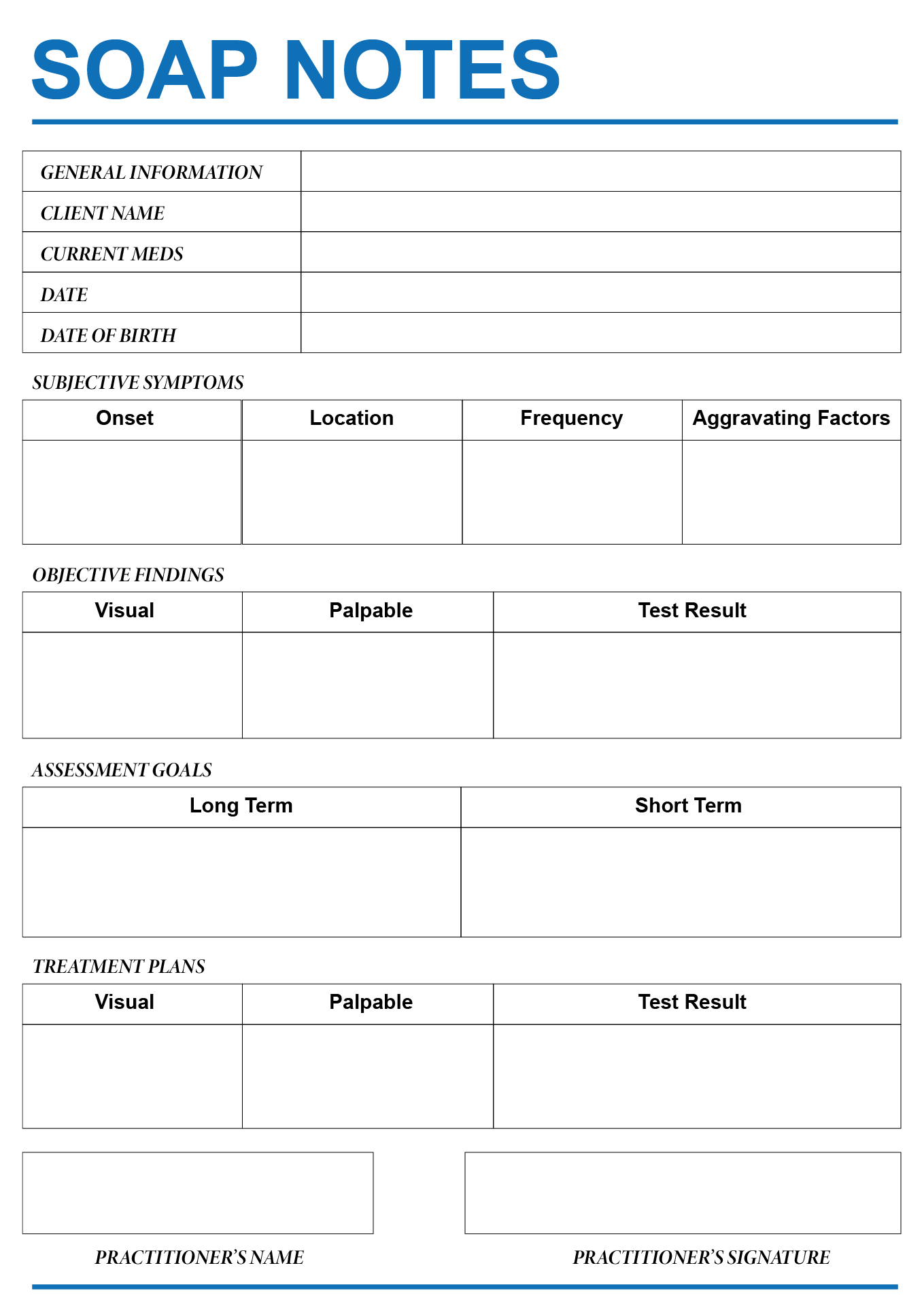
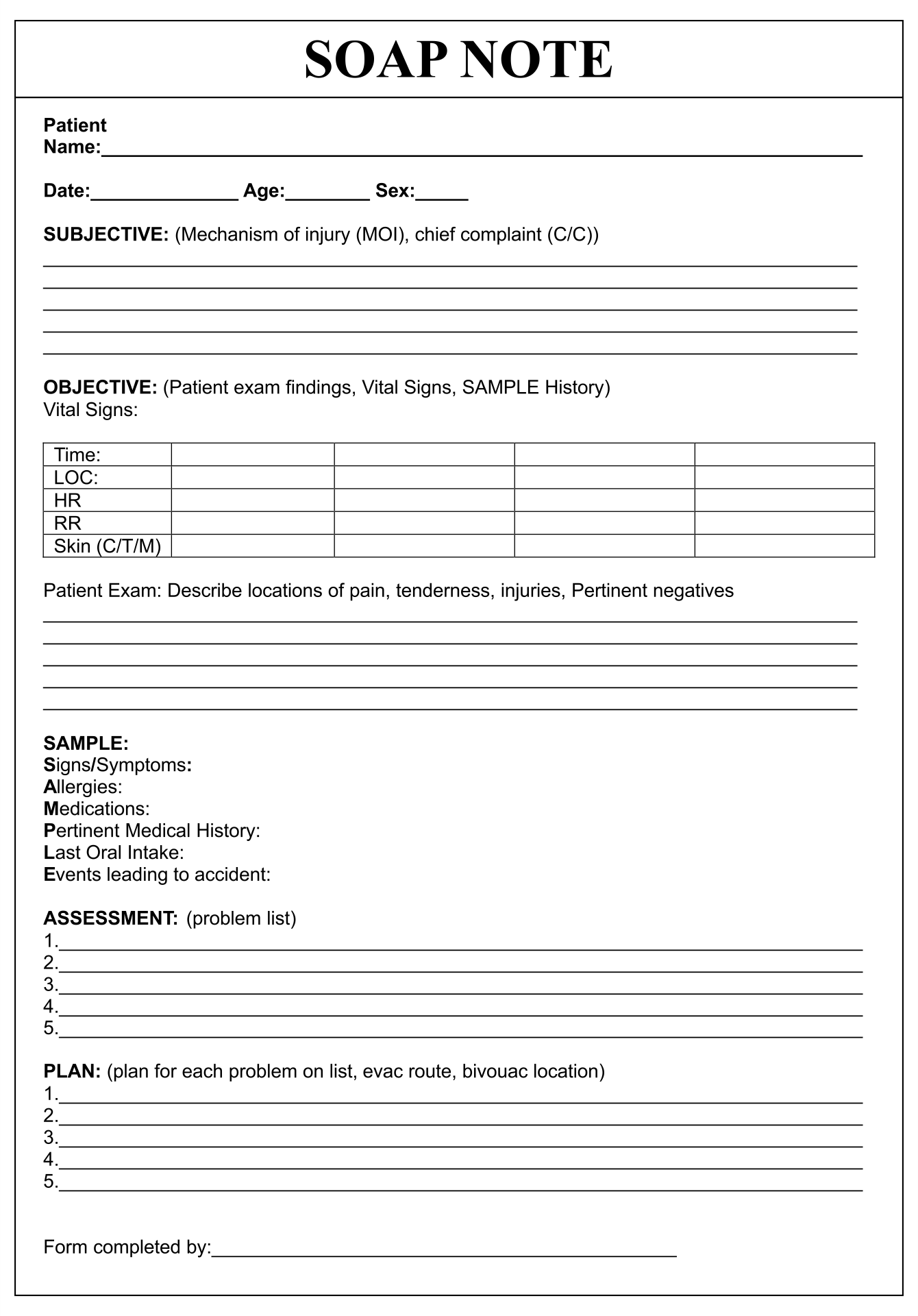
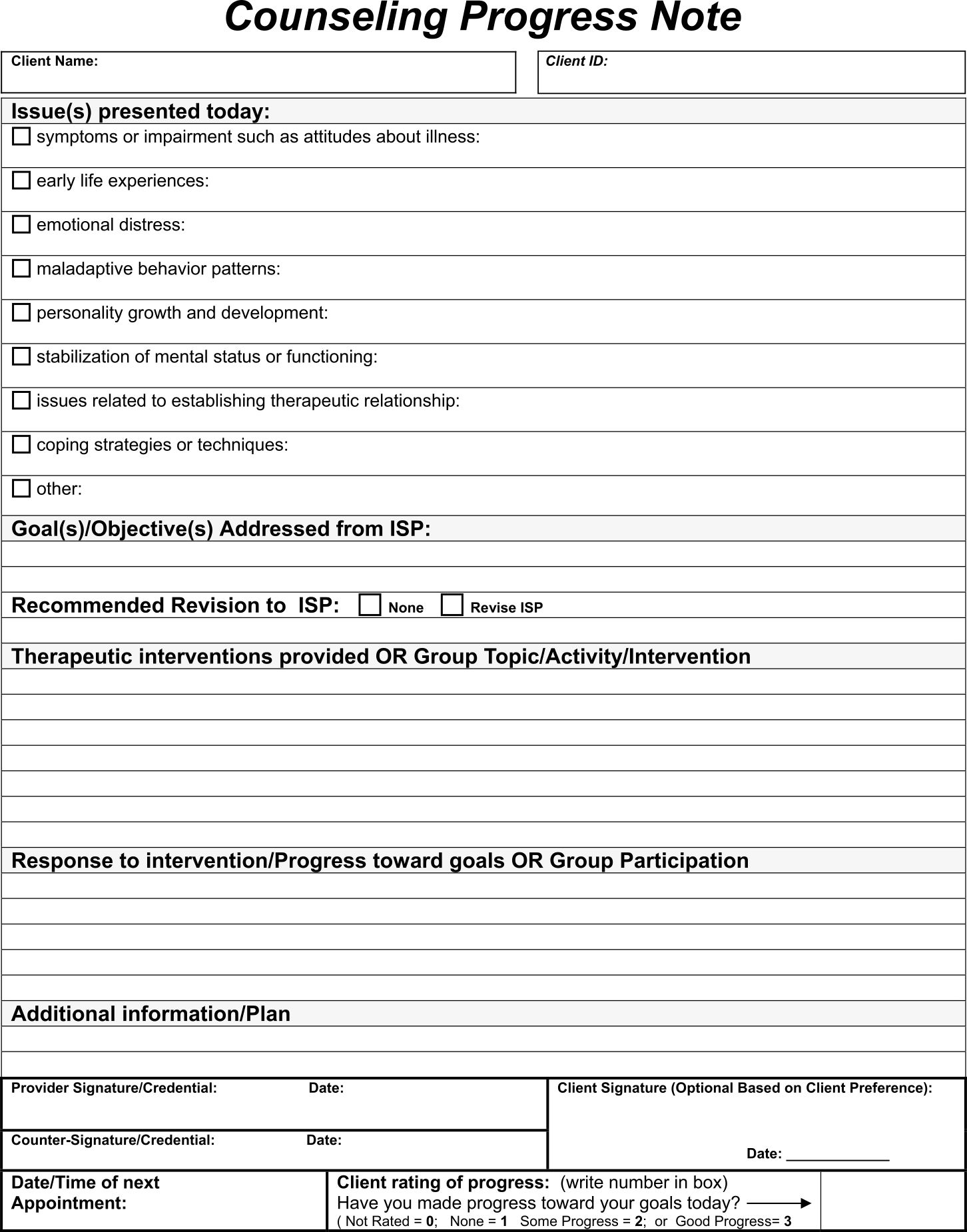
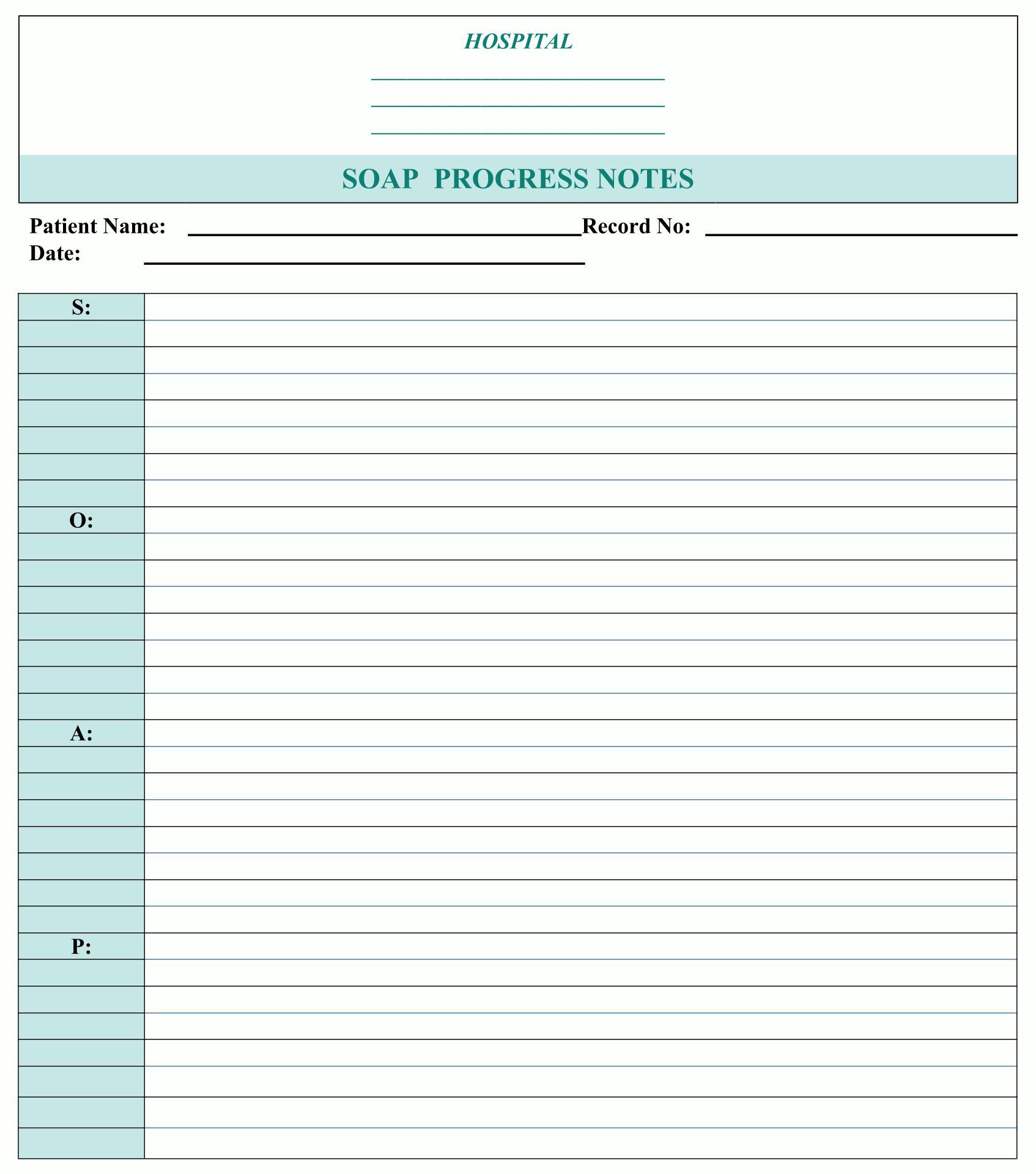
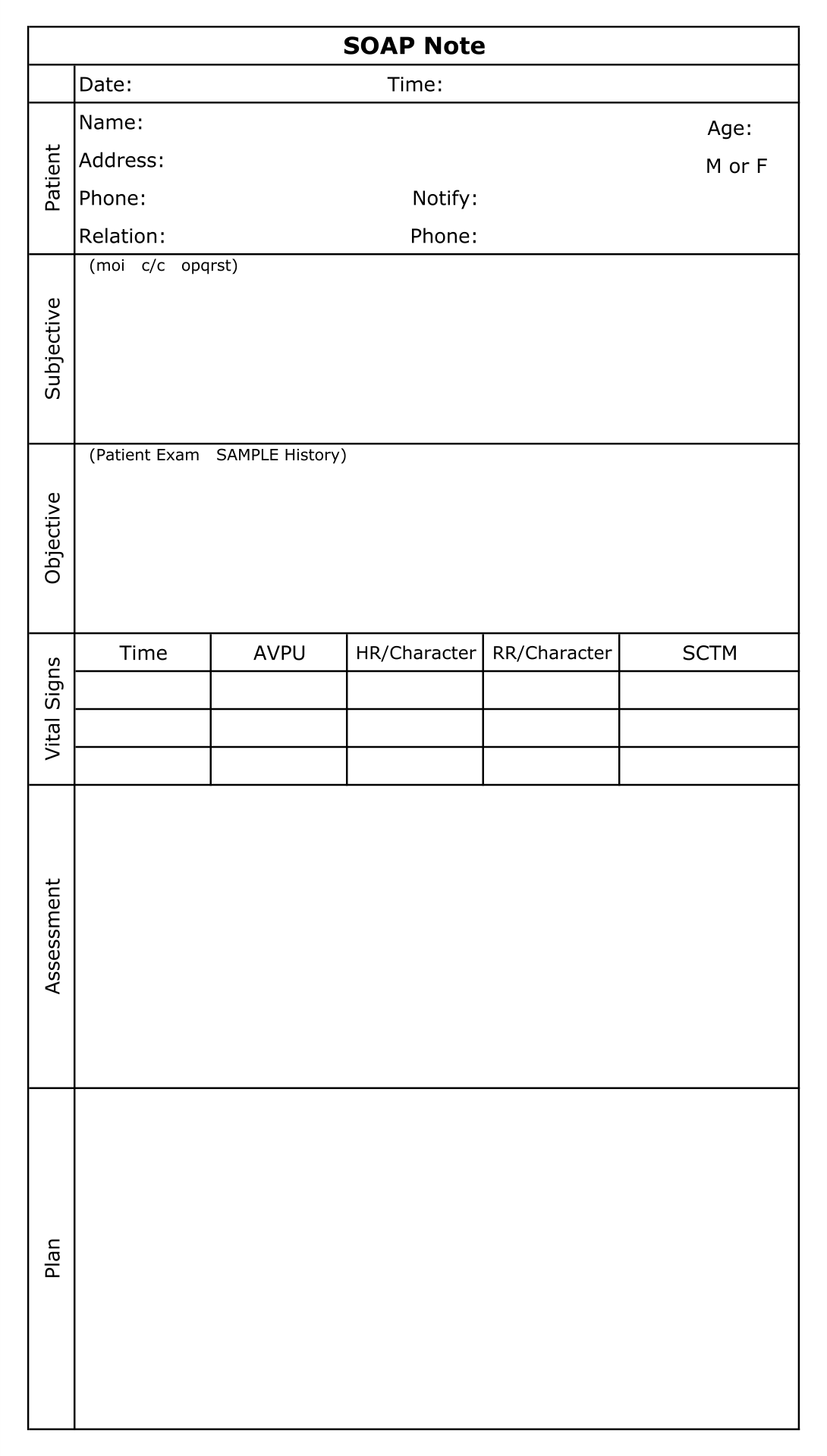
This template aids in creating methodical and structured notes during counseling sessions. It ensures all vital aspects of the session such as subjective observations, objective findings, the counselor's assessment, and the proposed plan are comprehensively documented. This not only enhances the effectiveness of your counseling by keeping your sessions organized but also improves client tracking over time.
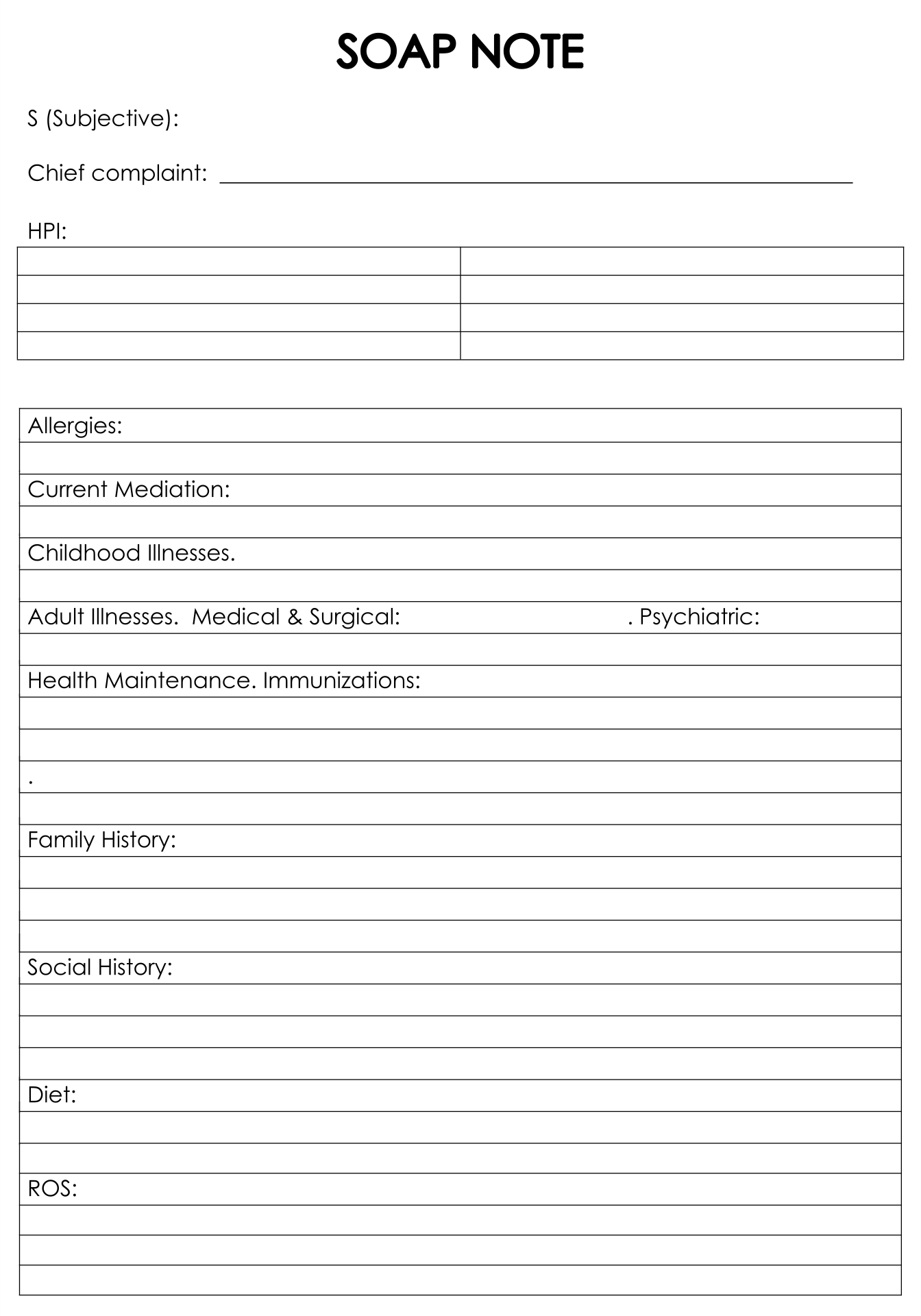
Using a sample SOAP note template can be a cornerstone for new and seasoned counselors alike, guiding you through the process of documenting sessions with precision. It provides a clear example of how to concisely record client encounters, ensuring you don't miss any critical information. This template can dramatically improve your documentation quality, making it easier to follow the client's progress.
A blank SOAP note template gives you the freedom to fill out client notes without constraints, customized to each session's unique needs. It ensures you capture the essential elements of each counseling session, paving the way for more effective client care. Your documentation process becomes streamlined, saving you time while maintaining high standards of record-keeping.
Have something to tell us?
Recent Comments
Printable counseling soap note templates offer therapists and counselors a practical and organized way to document their sessions, ensuring accurate record-keeping and streamlining the therapeutic process.
I found the Printable Counseling Soap Note Templates to be a helpful and practical tool in organizing my counseling sessions. It allows me to easily document important information and track progress with my clients. Thank you for providing such a useful resource!
I found the Printable Counseling Soap Note Templates to be incredibly helpful and user-friendly. They provide a convenient way to organize and document client progress during counseling sessions. Thank you for this valuable resource!